我的換腎後不幸感染記錄
棄趾保腎
棄趾保腎


一場惡夢,由一個長在左腳趾的水泡引起,再經一連串醫療失誤而導致:


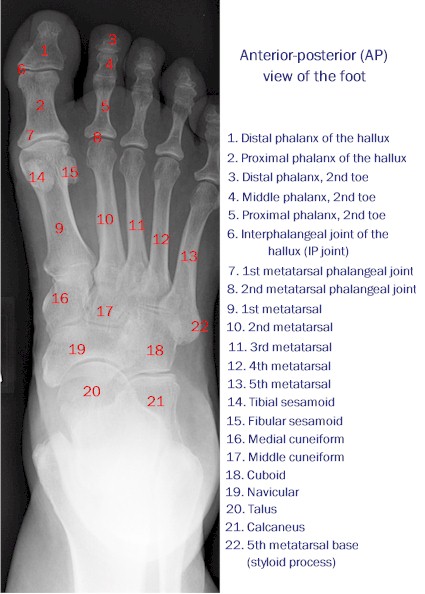
入院檢查後,証實因細菌感染入骨而患上「骨髓炎」 (Osteomyelitis)。須要吊消炎液 (強力抗生素) 治療四星期,看看效果如何。惟醫生恐怕強力抗生素或會導致新移植腎臟遭受排斥情況,醫生建議採用「棄趾保腎」治療策略。我為免夜長夢多,因小失大,決定接受!

手術後,因每天須要由護士揭開傷口紗布等候醫生驗查傷口,在等候期間,雖然有「無菌膠布」覆蓋,但存在空氣中的細菌早巳降悄悄地落在傷口表面了!結果感染了普遍存在醫院內的惡菌「綠膿桿菌」 (Pseudomonas Aeruginosa ) ,出院一週後,繼而須要再入院動手術清理部份 (5%)受感染的傷口!
出院後,左腳前掌仍然呈浮腫情況,足療師指示向醫生查詢。操刀醫生Dr Hung解譯左腳前掌仍然浮腫,全因傷口切得深而又須移除部份淋巴腺所致,待養傷一段時間後,其餘淋巴腺則可自行吸收瘀血及水份,而浮腫情況自消云!
住院治療
第一次住院治療記錄First Hospitalization Record
Alice Ho Miu Ling Nethersole Hospital
Admission Date: 04-03-2010 at 16:44Admission Source: A&ECase No: HN10008145(5)Specification: ORTWard: E2-29Diagnosis: Acute osteomyelitis, lower leg (left big toe)Infection: Osteomyelitis (骨髓炎)Procedure: Ray amputation of foot (left first ray)Procedure Date: 09-03-2010 at 15:30-16:30Spec: O&TClinician Name: KONG, Ming Fat BrianDischarge Date: 15-03-2010 Discharge Type: H+FUMedication on Discharge: AUGMENTIN Tablet 1g oral: 1000 mg bd for 1 week **single use**Follow up Clinic: ORT 22-03-2010 09:30 AHNMedical Officer In Charge: HUNG, Yuk WahSpecialist In Charge: FAN, Chi Ho
第二次住院治療記錄Second Hospitalization Record
Alice Ho Miu Ling Nethersole Hospital
Admission Date: 22-03-2010 11:50Admission Source: OPDCase No: HN10010597(4)Specification: ORTWard: E2-29Diagnosis: Post-operative wound infection
Infection: Pseudomonas Aeruginosa (綠膿桿菌)Because it thrives on most surfaces, this bacterium is found on and in medical equipment, causing cross infections in hospitals and clinics.Procedure: Excisional debridement of wound <5% of total body surface under general anaesthesia / MAC sedation
Excisional debridement is the definite cutting away of devitalized tissue, necrosis, or slough that includes cutting outside or beyond the wound margin.
An essential component of MAC sedation is the anesthesia assessment and management of a patient’s actual or anticipated physiological derangements or medical problems that may occur during a diagnostic or therapeutic procedure.Procedure Date: 26-03-2010 at 09:00-09:30Spec: O&TClinician Name: KONG, Ming Fat BrianDischarge Date: 07-04-2010 Discharge Type: H+FUMedication on Discharge: CIPROFLOXACIN HCL Tablet 1g oral: 750 mg bd prn (100%) for 1 week **single use**Follow up Clinic: ORT 24-05-2010 at 14:00 AHNMedical Officer In Charge: HUNG, Yuk WahSpecialist In Charge: FAN, Chi Ho
感染病菌第一次感染的病菌
骨髓炎 (Osteomyelitis)

病因
不論是何種情況,只要斷骨曝露在外面造成皮膚有開放性傷口就很容易讓病原有機會入侵內部造成骨髓炎。最常見的病例是因開放性骨折或外科手術引起的。亦有少數病例是患白血病的狗或其他有損及免疫機能的疾病會因為血液攜帶細菌或黴菌造成骨髓感染。

骨髓炎的症狀有跛行、發燒、骨病、連接骨頭到皮膚的竇管有滲出液。骨髓炎可用X光來確診,但治療上有一定困難。
治療
必先要瞭解造成骨髓炎的病原體才可以選擇最適合的抗生素作長期治療,若有骨塊壞死便必須動手術切除。

商品牌子名: AUGMENTIN TAB 1G
學名: Amoxycillin(阿莫西林)
藥理: 阿莫西林為一種廣譜青黴素,通過幹擾細菌細胞壁的生物合成而發揮抗菌作用,有效對抗大多數革蘭氏陽性及陰性細菌。克拉維酸鉀為β-內醯胺酶的不可逆性抑制劑,可保護阿莫西林,使其不因受多種革蘭氏陽性、陰性菌所產生的β-內醯胺酶破壞而喪失抗菌活性。
用途: 適用於細菌引起的下列感染:呼吸道感染如急慢性支氣管炎、大葉性及支氣管肺炎、膿胸、肺膿腫、耳鼻喉感染;生殖泌尿道感染如下泌尿道感染、膀胱炎、腎盂腎炎、盆腔感染、淋病、軟下疳;皮膚及軟組織感染如癤/膿腫、蜂窩組織炎、腹乞膿毒症;其他感染如骨髓炎、敗血症、腹膜炎、手術後感染。注射劑也適用於預防大手術後感染。
Osteomyelitis (骨髓炎)
Osteomyelitis is a bone infection usually caused by bacteria, including mycobacteria, but is sometimes caused by fungi.
Bacteria or fungi can infect bones by spreading through the bloodstream, spreading from nearby tissue, or directly invading the bone.
People have pain in one part of the bone, fever, and weight loss.
Blood tests and x-rays are done, and doctors remove a sample of bone for tests. Antibiotics are given for weeks, and surgery may be needed.
Osteomyelitis occurs most commonly in young children and in older people, but all age groups are at risk. Osteomyelitis is also more likely to occur in people with serious medical conditions.
When a bone becomes infected, the soft, inner part (bone marrow) often swells. As the swollen tissue presses against the rigid outer wall of the bone, the blood vessels in the bone marrow may become compressed, which reduces or cuts off the blood supply to the bone. Without an adequate blood supply, parts of the bone may die. These areas of dead bone are difficult to cure of infection because it is difficult for the body's natural infection-fighting cells and antibiotics to reach them. The infection can also spread outward from the bone to form collections of pus (abscesses) in adjacent soft tissues, such as the muscle.Causes
Bones, which usually are well protected from infection, can become infected through three routes:
* The bloodstream (which may carry an infection from another part of the body to the bones)
* Direct invasion (infection)
* Infections in adjacent bone or soft tissues
When organisms that cause osteomyelitis spread through the bloodstream, infection usually occurs in the ends of leg and arm bones in children and in the spine (vertebrae) in adults, particularly in older people. Infections of the vertebrae are referred to as vertebral osteomyelitis. People who undergo kidney dialysis and those who inject drugs using nonsterile needles are particularly susceptible to vertebral osteomyelitis.
Bacteria or fungal spores may infect the bone directly through open fractures, during bone surgery, or from contaminated objects that pierce the bone. Staphylococcus aureus is the bacteria most commonly responsible. Mycobacterium tuberculosis (the main cause of tuberculosis) can infect the vertebrae to cause osteomyelitis.
Osteomyelitis may also occur where a piece of metal has been surgically attached to a bone, as is done to repair hip or other fractures. Also, bacteria or fungal spores may infect the bone to which an artificial joint is attached. The organisms may be carried into the area of bone surrounding the artificial joint during the operation in which the joint is installed or the infection may occur later.
Osteomyelitis may also result from an infection in an adjacent soft tissue. The infection spreads to the bone after several days or weeks. This type of spread is particularly likely to occur in older people. Such an infection may start in an area damaged by an injury, radiation therapy, or cancer, or in a skin ulcer (particularly a foot ulcer) caused by poor circulation or diabetes. A sinus, gum, or tooth infection may spread to the skull.Symptoms
Infections of the leg and arm bones cause fever and, sometimes days later, pain in the infected bone. The area over the bone may be sore, warm, and swollen, and movement may be painful. The person may lose weight and feel tired.
Infections of the vertebrae usually develop gradually, causing persistent back pain and tenderness when touched. Pain worsens with movement and is not relieved by resting, applying heat, or taking analgesics. Fever, usually the most obvious sign of an infection, is often absent.
When osteomyelitis results from infections in adjacent soft tissues or direct invasion by an organism, the area over the bone swells and becomes painful. Abscesses may form in the surrounding tissue. These infections may not cause fever. Infection around an infected artificial joint or limb typically causes persistent pain in that area.
Chronic osteomyelitis may develop if osteomyelitis is not treated successfully. It is a persistent infection that is very difficult to eradicate. Sometimes, chronic osteomyelitis is undetectable for a long time, causing no symptoms for months or years. More commonly, chronic osteomyelitis causes bone pain, recurring infections in the soft tissue over the bone, and constant or intermittent drainage of pus through the skin. Such drainage occurs when a passage (sinus tract) forms from the infected bone to the skin surface and pus drains through the sinus tract.Diagnosis
Symptoms and findings during a physical examination may suggest osteomyelitis. For example, doctors may suspect osteomyelitis in a person who has persistent pain in part of a bone with or without a fever and feels tired much of the time.
Elevations in the erythrocyte sedimentation rate (ESR—a test that measures the rate at which red blood cells settle to the bottom of a test tube containing blood), and an elevated level of C-reactive protein (a protein that circulates in the blood and dramatically increases in level when there is inflammation) usually occur. Also, blood tests often indicate elevated levels of white blood cells. However, these blood tests are not sufficient to diagnose osteomyelitis.
An x-ray may show changes characteristic of osteomyelitis, but sometimes not until more than 3 weeks after the first symptoms occur. Computed tomography (CT) and magnetic resonance imaging (MRI) can also identify the infected area. However, these tests cannot always distinguish infections from other bone disorders. The infected area almost always appears abnormal on bone scans (images of bone made after injecting radioactive technetium), except in infants, because scans do not reliably indicate abnormalities in growing bones. White blood cell scans (images made after radioactive indium–labeled white blood cells are injected into a vein) can help distinguish between infection and other disorders in areas that are abnormal on bone scans.
To diagnose a bone infection and identify the organisms causing it, doctors may take samples of blood, pus, joint fluid, or the bone itself to test. Usually, for vertebral osteomyelitis, samples of bone tissue are removed with a needle or during surgery.Prognosis and Prevention
The prognosis for people with osteomyelitis is usually good with early and proper treatment. However, sometimes, chronic osteomyelitis develops, and a bone abscess may recur weeks to months or even years later.
Certain people who have artificial joints or metal components attached to a bone should take preventive antibiotics before surgery, including dental surgery, because these people may be at increased risk of infection from bacteria normally present in the mouth and other parts of the body. People can ask their health care practitioner for expert, detailed recommendations regarding preventive antibiotics. People undergoing surgical or dental procedures should tell their surgeon, orthopedist, or dentist that they have an artificial joint or metal component attached to a bone so that preventive antibiotics can be taken.Treatment
For children and adults who have recently developed bone infections through the bloodstream, antibiotics are the most effective treatment. If the bacteria causing the infection cannot be identified, then antibiotics that are effective against Staphylococcus aureus and many types of bacteria (broad-spectrum antibiotics are used. Depending on the severity of the infection, antibiotics may be given by vein (intravenously) for about 4 to 8 weeks but then may be given by mouth later. Some people need months of antibiotic treatment.
If a fungal infection is identified or suspected, antifungal drugs are required for several months. If the infection is detected at an early stage, surgery is usually not necessary.
For adults who have bacterial osteomyelitis of the vertebrae, the usual treatment is antibiotics for 6 to 8 weeks. Sometimes bed rest is needed, and the person may need to wear a brace. Surgery may be needed to drain abscesses or to stabilize affected vertebrae (to prevent the vertebrae from collapsing and thereby damaging nearby nerves, the spinal cord, or blood vessels).
When osteomyelitis results from an adjacent soft-tissue infection (such as in a foot ulcer caused by poor circulation or diabetes), treatment is more complex. Usually, all the dead tissue and bone are removed surgically, and the resulting empty space is packed with healthy bone, muscle, or skin. Then the infection is treated with antibiotics.
When an abscess is present, it usually needs to be drained surgically. Surgery may also be needed for people with persistent fever and weight loss.
Usually, an artificial joint that has an infection around it is removed and replaced. Antibiotics may be given several weeks before surgery to try to eradicate the infection, so that the contaminated artificial joint can be removed and a new one can be implanted at the same time. Rarely, treatment is not successful and the infection continues, requiring surgery to fuse the joint or amputate the limb.
第二次感染的病菌
綠膿桿菌 (Pseudomonas Aeruginosa)
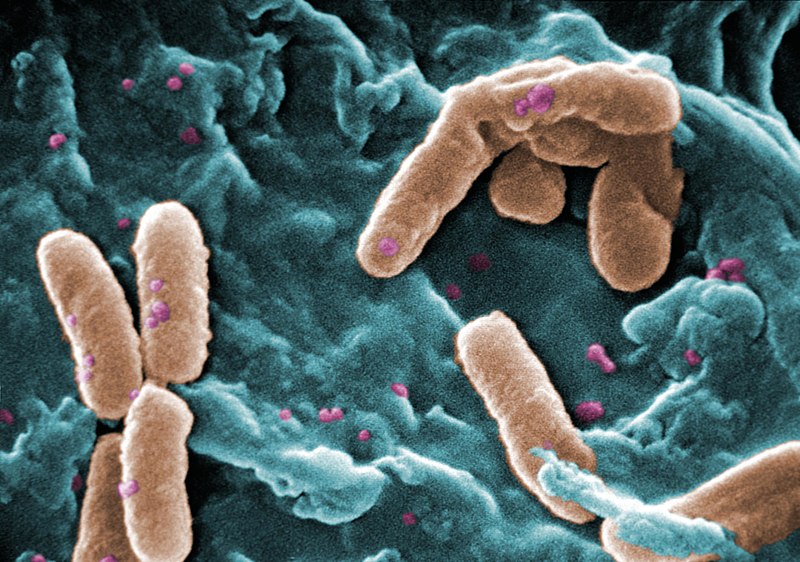
學名:綠膿桿菌,又稱銅綠假單胞菌,是一種革蘭氏陰性菌、好氧、呈長棒形的細菌,只有單向的運動性。牠是一種機會性感染細菌,且對植物亦是機會性感染的。
與其他假單胞菌屬的細菌一樣,綠膿桿菌分泌多種的色素,包括綠膿菌素(呈青色)、螢光素(呈螢光黃色)及綠膿菌紅素(呈啡紅色)。假單胞菌屬培養基P就是用作增加綠膿菌素及綠膿菌紅素的生產,而假單胞菌屬培養基F就是加強螢光素的生成。
綠膿桿菌的特徵是牠那如珠母般的外形及在試管內的葡萄氣味。臨床確認綠膿桿菌的方法是在於綠膿菌素及螢光素的生成,且在42℃的環境下生長的能力。綠膿桿菌在柴油及航空燃料中仍能生長,更被稱為「氫碳分解菌」,能引發微生物腐蝕作用。牠會產生一種暗色的凝膠墊,一般被誤解為藻類。
病因
綠膿桿菌是一種令免疫受損的機會性感染病原,一般影響肺部及泌尿道,或造成燒傷、傷口及其他血液感染,如敗血病。雖然很不常有,但綠膿桿菌亦會造成肺炎。在很多與通風機有關的肺炎研究中指出,綠膿桿菌是其中一種需要隔絕的細菌。綠膿菌素就是這種細菌的致病因子,且在氧化應激下能使秀麗隱桿線蟲死亡,但是有研究指水楊酸能抑制綠膿菌素的生成。10%在醫院感染的病症都是由綠膿桿菌所引致的。囊腫性纖維化病人的肺部是最先感染綠膿桿菌的一群。在缺乏適當處理食水質素下,牠亦是引致皮膚炎的其中一種細菌。牠也是造成燒傷感染最普遍的細菌。 治療
環丙氟哌酸,英文名Ciprofloxacin (INN),是一種氟喹諾酮類化合抗生素藥物。它是第二代氟喹諾酮抗菌素。它能殺死如炭疽一類的細菌,通過干擾導致DNA複製後反轉錄的酶,阻止DNA和蛋白質的合成。
在美國此藥被批准用於給成人治療以下已檢驗出的病菌感染:
l 皮膚和皮膚結構感染
l 骨和關節感染
治療日程及養傷記錄
2010年1月
|
星期日
|
星期一
|
星期二
|
星期三
|
星期四
|
星期五
|
星期六
|
| 1 | 2 | |||||
| 3 | 4 | 5 | 6/1 | 7 | 8 左腳趾 起水泡  用早前足療師間出之SODIUM CHLORIDE 0.9% IRRIGATION SOLUTION (生理鹽水)自行在家洗傷口。 |
9 自行在家 洗傷口。 |
10 自行在家洗傷口。 |
11 自行在家 洗傷口。 |
12 北區醫院 足病覆診 11:00 am  IODINE SOLUTION CHLORHEXIDINE 0.05% ANTISEPTIC SOLUTION |

洗傷口。
13/1

自行在家
洗傷口。

自行在家
洗傷口。

自行在家
洗傷口。

自行在家
洗傷口。

自行在家
洗傷口。

自行在家
洗傷口。

北區醫院
足病覆診
11:00 am

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

那打素
抽血

大埔診所洗左腳趾傷口
$17.00

北區醫院
足病覆診
11:00 am

那打素
腎科覆診
11:00 am
CR 94
FK 5.2

大埔診所
洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00

大埔診所洗左腳趾傷口
$17.00
2010年2月
星期日
|
星期一
|
星期二
|
星期三
|
星期四
|
星期五
|
星期六
|
1 大埔診所洗左腳趾傷口 $17.00 |
2 北區醫院 足病覆診 12:00 am |
3/2 |
27 大埔診所洗左腳趾傷口 $17.00 | |||
28 大埔診所洗左腳趾傷口 $17.00 |
星期日
|
星期一
|
星期二
|
星期三
|
星期四
|
星期五
|
星期六
|
1 大埔診所洗左腳趾傷口 $17.00 |
2 大埔診所洗左腳趾傷口 $17.00  照腎X光 11:00 am |
3/3 大埔診所洗左腳趾傷口 $17.00 |
4 北區醫院 足病覆診 11:00 am  住那打素 |
5 住那打素醫院骨科 E2-29床 |
6 住那打素醫院骨科 E2-29床 | |
7 住那打素醫院骨科 E2-29床 |
8 住那打素醫院骨科 E2-29床  |
9 住那打素醫院骨科 E2-29床  截趾手術 半身麻醉3:30 – 4:30 pm |
10/3 住那打素醫院骨科 E2-29床 |
11 住那打素醫院骨科 E2-29床 |
12 住那打素醫院骨科 E2-29床 |
13 住那打素醫院骨科 E2-29床 |
14 住那打素醫院骨科 E2-29床 |
15 住那打素醫院骨科 E2-29床  3:00 pm   體重:76Kg |
16    |
17/3    |
18     大埔診所洗左腳趾傷口 $17.00 |
19     大埔診所洗左腳趾傷口 $17.00 |
20     大埔診所洗左腳趾傷口 $17.00 |
21     大埔診所洗左腳趾傷口 $17.00 |
22     那打素 骨科覆診 9:30 am  傷口因受感染: 體重:78Kg |
23 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
24/3 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
25 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
26 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床  重做手術 清洗傷口 半身麻醉 9:00 – 9:30 am |
27 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 打開傷口紗布後,發現左腳前掌浮腫 |
28 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
29 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
30 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
31/3 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
星期日
|
星期一
|
星期二
|
星期三
|
星期四
|
星期五
|
星期六
|
1 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
2 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
3 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 | ||||
4 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
5 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
6 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床 |
7/4 傷口因受感染:Pseudomonas Aeruginosa (綠膿桿菌) 再住那打素醫院骨科 E2-29床  那打素 腎科覆診 11:30 am 腎科主管醫生Dr Yue恐怕抗生素影响腎功能,特安排兩星期後抽血覆診    開出口服抗生素:Cipprofloxacin HCL TabletORAL 750mg bd pm (100%) for 1 week |
8   |
9   |
10   |
11   |
12 1318 - 829    那打素 骨科覆診 9:30 am  拆線  左腳前掌仍然浮腫,再開出抗生素:Cipprofloxacin HCL TabletORAL 750mg bd pm (100%) for 1 week |
13   |
14/4   |
15   |
16   |
17   |
18   |
19    那打素 抽血: Anti-HBs Anti-HCV Bone Profile, Plasma CBC with WBC Differential (CBP) FK506 Glucose Fasting, plasma HBsAg LFT Lipid profile (TC,TG,HDL) fasting Parathyroid Hormone, plasma RFT 心電圖 X光: Chest, PA  足病覆診 3:00 pm左腳前掌仍然浮腫,足療師指示在換腎覆診時,向醫生查詢。   |
20   |
21/4   停服抗生素:Cipprofloxacin HCL Tablet |
22   |
23    那打素 腎科覆診 11:00 am CR 99 標準 FK 6.1 標準腎科主管醫生Dr Yue恐怕抗生素影响腎功能,特安排三星期後抽血覆診 左腳前掌仍然浮腫,主診Dr Yue指示往D2骨科日間護理中心Walk-in急診。  那打素 骨科覆診 2:30 pm Walk-in D2急診,主刀醫生Dr Hung指左腳前掌仍然浮腫全因傷口切得深而又須移除大部份淋巴腺所致,假以時日則可自行吸收瘀血水而消腫矣!  CHLORHEXIDINE ACETATE 0.015% + CETRIMIDE 0.15% 1 LITRE  洗傷口。 |
24   |
25   |
26   |
27   |
28/4   |
29    那打素 眼科覆診 9:30 am |
30   |
2010年5月
星期日
|
星期一
|
星期二
|
星期三
|
星期四
|
星期五
|
星期六
|
1   | ||||||
2   |
3    浸會醫院 骨科初診 10:00 am |
4   |
5/5   |
6   |
7   |
8   |
9   |
10    那打素 抽血:  足病覆診 10:30 am |
11   |
12/5   |
13   |
14    那打素醫院 腎科覆診 11:00 am |
15   |
16   |
17   |
18   |
19/5   |
20    那打素 抽血: LFT RFT ESR FK 506 C-Reactive Protein CBC with WBC |
21 1357 - 868    體重:74Kg162.8 LB |
22   |
23   |
24    那打素 X光 12:30 pm  那打素 骨科覆診 2:00 pm |
25   |
26//5   |
27   |
28   |
29   |
30   |
31   |
今天(3/5/2010)是第二次手術後第38天(26/3/2010至 3/5/2010) ,左腳掌仍然有點紅腫,由於那打素骨科覆診是月尾24/5/2010,為免在缺乏醫療指示下,耽擱康服進度,所以决定今天早上10:00前住 浸會醫院 專科門診部 向 骨科 魏偉奇醫生 (Dr Ngai Wai Kee, Wilkie) 求診。經檢查後,他說以臨床經驗來判斷,再經電子病歷顯示之血液檢驗數值作佐證,不像是發炎情況。可能是外傷手術之後,局部血液或淋巴循環不良而引起的。他再指出另一個重點:血液是由心臟泵往腳趾尖端,回流則須靠運動助長血液循還的!祇要放胆讓左腳受點力,多行兩步,紅腫自然消退!此話不爽,在回家路上,我讓左腳多受點力,紅腫情況果然得以改善!
病情佐證 之 血液檢驗數值
ALP (鹼性磷酸酵素)http://www.labtestsonline.org/understanding/analytes/alp/ask.php
Also known as: ALK PHOS; Alkp
Formal name: Alkaline Phosphatase
Related tests: AST; ALT; GGT; Bilirubin; Liver panel; 5'-nucleotidase; Bone markers; Alkaline phosphatase isoenzymes; Bone specific ALP
鹼性磷酸酵素 (Alkaline Phosphatase, ALP) 是人體的一種酵素,普遍存在於全身細胞中,其中以肝、膽、骨骼中含量最多,因為ALP對肝膽的異常較敏感,所以當這些器官的細胞受傷時,ALP數值即升高。但正值發育期間的小孩或青少年,其值雖可高達2、3倍以上,但仍屬正常。ALP數值偏高時可能為急性肝炎、膽道結石、肝內膽汁滯留、肝硬化、肝膽腫瘤、骨病變或骨癌等(參考值30 – 120 units/L)。
04 March 2010 ALP: 330 units/L (參考值30 – 120 units/L)
19 April 2010 ALP: 112 units/L (參考值30 – 120 units/L)ò
At a Glance
Why Get Tested?
To screen for or monitor treatment for a liver or bone disorder
When to Get Tested?
As part of a routine liver panel or when a person has symptoms of a liver or bone disorder
Sample Required?
A blood sample drawn from a vein in the arm
Test Preparation Needed?
Fasting is preferred but not required for this test.
The Test
How is it used?
The alkaline phosphatase test (ALP) is used to help detect liver disease or bone disorders. In conditions affecting the liver, damaged liver cells release increased amounts of ALP into the blood. This test is often used to detect blocked bile ducts because ALP is especially high in the edges of cells that join to form bile ducts. If one or more of them are obstructed, for example by a tumor, then blood levels of ALP will often be high.
Any condition that affects bone growth or causes increased activity of bone cells can affect ALP levels in the blood. An ALP test may be used, for example, to detect cancers that have spread to the bone or to help diagnose Paget's disease. This test may also sometimes be used to monitor treatment of Paget's disease or other bone conditions, such as vitamin D deficiency.
If ALP results are increased but it is not clear whether this is due to liver or bone disease, then tests for ALP isoenzyme tests may be done to determine the cause. A GGT test and/or a test for 5'-nucleotidase may also be done to differentiate between liver and bone disease. GGT and 5'-nucleotidase levels are increased in liver disease but not bone disorders.
When is it ordered?
ALP may be ordered as part of a routine lab testing profile, often with a group of other tests called a liver panel. It is also usually ordered along with several other tests when a person has symptoms of a liver or bone disorder.
Signs and symptoms of liver involvement may include:
· Weakness, fatigue
· Loss of appetite
· Nausea, vomiting
· Abdominal swelling and/or pain
· Jaundice
· Dark urine, light colored stool
· Itching (pruritis)
Some examples of the signs and symptoms suggesting a bone disorder include:
· Bone and/or joint pain
· Increased frequency of fractures
· Deformed bones
· What does the test result mean?
· High ALP usually means that either the liver has been damaged or a condition causing increased bone cell activity is present. If other liver tests such as bilirubin, aspartate aminotransferase (AST), or alanine aminotransfere (ALT) are also high, usually the ALP is coming from the liver. If calcium and phosphate measurements are abnormal, usually the ALP is coming from bone. If a GGT or 5'-nucleotidase is also increased, then the high ALP is likely due to liver disease. If either of these two tests is normal, then the high ALP is likely due to a bone condition.
· If it is not clear from signs and symptoms or from other routine tests whether the high ALP is due to liver or bone, then a test for ALP isoenzymes may be necessary to distinguish between bone and liver ALP.
· ALP in Liver disease
ALP results are usually evaluated along with other tests for liver disease. In some forms of liver disease, such as hepatitis, ALP is usually much less elevated than AST and ALT. When the bile ducts are blocked (usually by gallstones, scars from previous gallstones or surgery, or by cancers), ALP and bilirubin may be increased much more than AST or ALT. It may also be increased in liver cancer.
· ALP in Bone disease
In some bone diseases, such as Paget's disease, where bones become enlarged and deformed, or in certain cancers that spread to bone, ALP may be increased.
· If a person is being successfully treated for Paget's disease, then ALP levels will decrease or return to normal over time. If someone with bone or liver cancer responds to treatment, ALP levels should decrease.
· Low levels of ALP may be seen temporarily after blood transfusions or heart bypass surgery. A deficiency in zinc may cause decreased levels. A rare genetic disorder of bone metabolism called hypophosphatasia can cause severe, protracted low levels of ALP.
· Is there anything else I should know?
· Pregnancy can increase ALP levels. Temporary elevations are also seen with healing fractures.
· Children and adolescents normally have higher ALP levels than adults because their bones are growing, and ALP is often very high during a growth spurt, which occurs at different ages in boys and girls.
· Some drugs may affect ALP levels. For example, oral contraceptives may decrease levels while anti-epileptics may increase levels.
The Test Sample
What is being tested?
· Alkaline phosphatase (ALP) is an enzyme found in several tissues throughout the body, including liver, bone, kidney, bowel (intestine), and in the placenta of women who are pregnant. However, the highest concentrations ALP are present in the cells that comprise the bone and liver. In the liver, it is found on the edges of cells that join to form bile ducts - tiny tubes that drain bile from the liver to the bowels where it is needed to help digest fat in the diet. ALP in bone is produced by special cells called "osteoblasts" that are involved in the formation of bone. Each of the various tissue types produces distinct forms of ALP called isoenzymes.
· Elevated levels of ALP in the blood are most commonly caused by liver disease or bone disorders. Levels of the enzyme can be greatly increased, for example, in cases where one or more bile ducts are blocked. Smaller increases of blood levels are seen in liver cancer and cirrhosis, with use of drugs toxic to the liver, and in hepatitis. Any condition causing excessive bone formation, including bone disorders such as Paget's disease and others such as rheumatoid arthritis and healing fractures, can cause increased ALP levels. Children and adolescents typically have higher blood ALP levels because their bones are still growing.
· It is possible to distinguish between the different forms (isoenzymes) of ALP produced by different types of tissues in the body. If it is not apparent from clinical signs and symptoms whether the source of a high ALP test result is from liver or bone disease, then a test may be performed to determine which isoenzyme is increased in the blood. This can help establish whether the increase is due to bone or liver disease.
How is the sample collected for testing?
· A blood sample is taken by needle from a vein in the arm.
· NOTE: If undergoing medical tests makes you or someone you care for anxious, embarrassed, or even difficult to manage, you might consider reading one or more of the following articles: Coping with Test Pain, Discomfort, and Anxiety, Tips on Blood Testing, Tips to Help Children through Their Medical Tests, and Tips to Help the Elderly through Their Medical Tests.
· Another article, Follow That Sample, provides a glimpse at the collection and processing of a blood sample and throat culture.
· Is any test preparation needed to ensure the quality of the sample?
· Fasting is preferred but not required for this test. Eating a meal can increase the ALP level slightly for a few hours in some people. It is usually better to do the test after fasting overnight. In this case, only water is permitted.
Common Questions
1. What other tests are used to evaluate liver disorders?
Other commonly used liver tests include more enzymes found in liver cells, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST). A test for bilirubin, a substance produced by the breakdown of red blood cells and removed from the body by the liver, may also be done. Sometimes these tests are performed together as a liver panel.
2. Who is at risk for liver disease and/or damage?
Some of those who are at risk of liver disease include the following:
· People who have been exposed to hepatitis viruses
· Heavy drinkers
· People who take medication that can be toxic to the liver or who are exposed to other liver toxins
· Those who are obese, have metabolic syndrome or insulin resistance
· People with an inherited disorder affecting the liver such as Wilson's disease or hemachromatosis
See the article on Liver Disease for more on these.
3. What other laboratory tests may be done if I have a bone disorder?
Depending on the cause, your condition may be diagnosed and/or monitored using other tests such as calcium, phosphorus, vitamin D, or bone markers - a group of tests used to measure bone formation and bone resorption.
C-Reactive Protein (C反應蛋白)http://www.labtestsonline.org/understanding/analytes/crp/test.html
Also known as: CRP
Formal name: C-Reactive Protein
Related tests: High-sensitivity C-reactive protein (hs-CRP); Erythrocyte sedimentation rate (ESR)
C反應蛋白(C-Reactive Protein, CRP)會出現於各種發炎性疾病。體內發炎時,除CRP 值會增加,白血球數目及ESR 值也會升高。正常人其數值是很低的,有發炎之病患其報告為數值升高(參考值0 – 0.5 mg/dL)。
At a Glance
Why Get Tested?
To identify the presence of inflammation and to monitor response to treatment [Note: to test for your risk of heart disease, a more sensitive test (hs-CRP) is used.]
When to Get Tested?
When your doctor suspects that you might be suffering from an inflammatory disorder (as with certain types of arthritis and autoimmune disorders or inflammatory bowel disease) or to check for the presence of infection (especially after surgery)
Sample Required?
A blood sample taken from a vein in your arm
The Test
How is it used?
The CRP test is useful in assessing patients with:
· Inflammatory bowel disease
· Some forms of arthritis
· Autoimmune diseases
· Pelvic inflammatory disease (PID)
CRP may be used to screen apparently healthy people for the following conditions. However, in these cases, the more sensitive test hs-CRP will be ordered:
· Coronary heart disease (CHD)
· Cardiovascular disease
While the CRP test is not specific enough to diagnose a particular disease, it does serve as a general marker for infection and inflammation, thus alerting medical professionals that further testing and treatment may be necessary.
When is it ordered?
Because CRP increases in severe cases of inflammation, the test is ordered when acute inflammation is a risk (such as from an infection after surgery) or suspected based on patient symptoms. It is also ordered to help evaluate conditions such as rheumatoid arthritis and lupus and is often repeated to determine whether treatment is effective. This is particularly useful for inflammation problems since CRP levels drop as inflammation subsides.
CRP also is used to monitor wound healing and to monitor patients who have surgical cuts (incisions), organ transplants, or burns as an early detection system for possible infections.
What does the test result mean?
A high or increasing amount of CRP in your blood suggests that you have an acute infection or inflammation.
If the CRP level in your blood drops, it means that you are getting better and inflammation is being reduced.
Is there anything else I should know?
CRP levels can be elevated in the later stages of pregnancy as well as with use of birth control pills or hormone replacement therapy (i.e., estrogen). Higher levels of CRP have also been observed in the obese.
Another test to monitor inflammation is called the erythrocyte sedimentation rate (ESR). Both tests are elevated in the presence of inflammation; however, CRP appears and then disappears sooner than changes in the ESR. Thus, your CRP level may fall to normal if you have been treated successfully, such as for a flare-up of arthritis, but your ESR may still be abnormal for a while longer.
The Test Sample
What is being tested?
C-reactive protein (CRP) is an acute phase reactant, a substance made by the liver and secreted into the bloodstream within a few hours after the start of an infection or inflammation. Increased levels are observed after a heart attack, in sepsis, and after a surgical procedure. Its rise in the blood can also precede pain, fever, or other clinical indicators. The level of CRP can jump a thousand-fold in response to inflammation and can be valuable in monitoring disease activity.
How is the sample collected for testing?
A blood sample is obtained by inserting a needle into a vein in your arm.
NOTE: If undergoing medical tests makes you or someone you care for anxious, embarrassed, or even difficult to manage, you might consider reading one or more of the following articles: Coping with Test Pain, Discomfort, and Anxiety, Tips on Blood Testing, Tips to Help Children through Their Medical Tests, and Tips to Help the Elderly through Their Medical Tests.
Another article, Follow That Sample, provides a glimpse at the collection and processing of a blood sample and throat culture.
Is any test preparation needed to ensure the quality of the sample?
No test preparation is needed.
Common Questions
1. What are chronic inflammatory diseases?
"Chronic inflammatory diseases" is a non-specific term used to characterize long-lasting or frequently recurring bouts of inflammation as associated with a more specific disease. This can be caused by a number of different pathological conditions such as arthritis, lupus, or inflammatory bowel disease (Crohn’s disease).
2. What is the difference between regular CRP and hs-CRP tests?
Both tests measure the same molecule in the blood. The high sensitivity CRP (hs-CRP) test measures very small amounts of CRP in the blood and is ordered most frequently for seemingly healthy people to assess their potential risk for heart problems. It measures CRP in the range from 0.5 to 10 mg/L. The regular CRP test is ordered for patients at risk for infections or chronic inflammatory diseases (see Question #1). It measures CRP in the range from 10 to 1000 mg/L.
White Blood Cell (白血球)
Differential Count
http://www.labtestsonline.org/understanding/analytes/differential/glance.html
Also known as: Leukocyte differential count; Peripheral differential; White blood cell morphology; WBC differential; Diff
Formal name: White Blood Cell Count Differential
Related tests: Complete blood count; Blood smear
白血球是免疫系統的主要成員,白血球在人體中俱有重要的防禦功能,係由骨髓製造而後巡迴在血液及組織器官內執行巡邏捍衛任務。白血球可因感染症、發炎、過敏、腫瘤、自體免疫疾病、組織壞死、物理性刺激、情緒反應或藥物之影響等原因升高。白血球高,反映免疫系統在活動,即身體出現問題。假若低過正常的白血球數(參考值3200 – 9800 cell/mm3),即代表患上白血球減少症。白血球減少或白血球功能缺損都會使身體抵抗致病菌的能力下降,身體就容易受感染生病。
At a Glance
Why Get Tested?
To diagnose an illness affecting your immune system, such as an infection or viral condition, or other diseases that affect your white blood cells, such as leukemias
When to Get Tested?
As part of a complete blood count (CBC), which may be ordered for a variety of reasons
Sample Required?
A blood sample drawn from a vein in your arm or by a fingerstick (children and adults) or heelstick (infants)
Test Preparation Needed?
None
The Test
How is it used?
The white blood cell differential assesses the ability of the body to respond to and eliminate infection. It also detects the severity of allergic and drug reactions plus the response to parasitic and other types of infection. It is essential in evaluating the reaction to viral infections and response to chemotherapy. It can also identify various stages of leukemia.
When is it ordered?
The white blood cell differential is normally run as part of the complete blood count (CBC), which is ordered for many different reasons.
What does the test result mean?
The results indicate the percentage of each type of white blood cell that is present.
Neutrophils can increase in response to bacterial infection or inflammatory disease. Severe elevations in neutrophils may be caused by various bone marrow disorders, such as chronic myelogenous leukemia. Decreased neutrophil levels may be the result of severe infection or other conditions, such as responses to various medications, particularly chemotherapy.
Eosinophils can increase in response to allergic disorders, inflammation of the skin, and parasitic infections. They can also increase in response to some infections or to various bone marrow disorders. Decreased levels of eosinophils can occur as a result of infection.
Basophils can increase in cases of leukemia, chronic inflammation, the presence of a hypersensitivity reaction to food, or radiation therapy.
Lymphocytes can increase in cases of viral infection, leukemia, cancer of the bone marrow, or radiation therapy. Decreased lymphocyte levels can indicate diseases that affect the immune system, such as lupus, and the later stages of HIV infection.
Monocyte levels can increase in response to infection of all kinds as well as to inflammatory disorders. Monocyte counts are also increased in certain malignant disorders, including leukemia. Decreased monocyte levels can indicate bone marrow injury or failure and some forms of leukemia.
Since percentages might be misleading in some patients, absolute values of the various types of WBCs can also be reported, such as the absolute neutrophil count (ANC), also known as the absolute granulocyte count or AGC. Absolute values are calculated by multiplying the number of WBCs by the percentage of each type of white cell and can aid in diagnosing illness and monitoring therapy.
Is there anything else I should know?
Eating, physical activity, and stress may alter white blood cell differential values.
Long-term use of steroids or long-term exposure to toxic chemicals (such as lye or insecticides) can increase the risk of an abnormal differential.
Common Questions
1. What are the individual functions of each type of white blood cell?
· Neutrophils, the most common white blood cells, are infection-fighters that increase during bacterial or fungal infections.
· Lymphocytes are responsible for the immune response and regulation of antibody production. They are increased in some leukemias.
· Monocytes are another type of phagocyte that ingests foreign cells. These may increase in some leukemias (different types from those that increase the lymphocytes).
· Eosinophils are a type of phagocyte that increases during allergic attacks and some parasitic infestations.
· Basophils control inflammation and damage to the body. They increase in some blood diseases and poisoning.
2. What are other names for neutrophils that might appear on a lab report?
Neutrophils are also known as granulocytes (grans), polys, PMNs, or segs.
The Test Sample
What is being tested?
There are five types of white blood cells, each with different functions: neutrophils, lymphocytes, monocytes, eosinophils and basophils. The differential reveals if these cells are present in normal proportion to one another, if one cell type is increased or decreased, or if immature cells are present. This information is helpful in diagnosing specific types of illnesses that affect the immune system.
White blood cells are made in your bone marrow. They protect your body against infection and aid your immune system. If an infection develops, white blood cells attack and destroy the microorganism causing the infection.
How is the sample collected for testing?
The test is performed on a blood sample drawn from a vein in the arm or from a fingerstick (for children and adults) or heelstick (for infants).
NOTE: If undergoing medical tests makes you or someone you care for anxious, embarrassed, or even difficult to manage, you might consider reading one or more of the following articles: Coping with Test Pain, Discomfort, and Anxiety, Tips on Blood Testing, Tips to Help Children through Their Medical Tests, and Tips to Help the Elderly through Their Medical Tests.
Another article, Follow That Sample, provides a glimpse at the collection and processing of a blood sample and throat culture.
Is any test preparation needed to ensure the quality of the sample?
No test preparation is needed.
病房膳食
特別餐:免 (牛肉) 、糖尿控制、低熱量 1500 kcal、低鈉 2g、低磷、低鉀
免 (牛肉) - 好讓傷口早點癒合。
低鈉 - 避免體內積水及控制血壓。
低磷 - 避免皮膚痕癢,所以無魚吃!
低鉀 - 避免血鉀過高,所以無深綠色蔬菜吃!
早餐:粥
曾經吃過的粥品:
低鹽碎豬粥
低鹽魚蓉粥
低鹽豬肉紅米粥低鹽免治雞胸肉粥低鹽冬菇免治雞胸肉粥
低鹽粟米免治雞胸肉粥
午餐:飯 + 菜 + 肉
晚餐:飯 + 菜 + 肉 + 小蘋果
正飯 (平飯碗 - 5S)曾經吃過的蔬菜類:
西芹
冬瓜
唐生菜
節瓜片
烚甘筍條
曾經吃過的肉類小菜:羅漢上素 (180 gm)醬爆肉片(180 gm)豉椒肉片 (180 gm)葡汁雞球 (180 gm)
芋頭炆雞球 (180 gm)
豉椒汁梅肉粒 (180 gm) 洋葱燒汁雞球 (150 gm)火腿冬菇肉片 (180 gm)冰梅子薑雞球 (180 gm)法邊豆汁肉片 (180 gm)
匈牙利汁雞球 (180 gm)蕃茄青豆草菇雞球 (180 gm)機攪葡汁免治豬肉 (120 gm)珍珠豆卜豆豉汁肉片 (180 gm)青紅椒白菌白汁雞球 (180 gm)草菇蟹柳蛋花汁雞球 (180 gm)青紅椒白菌白汁肉片 (180 gm)











兒女們送的心意

沒有留言:
張貼留言